When deciding whether to donate, it is important to understand all of the possible medical, psychological, and financial risks. It is okay for the donor to stop pursuing living donation at any point if they decide that it is not the right decision.
Transplant options: Deceased or living donation?
What is a deceased donor kidney transplant?
This is a surgery where doctors put a kidney from someone who has died into someone whose kidneys no longer work.
What is a living donor kidney transplant?
This is a surgery where doctors put a kidney from a living person into someone whose kidneys no longer work. A transplant from a living donor may be the best option for most people who need a kidney transplant because these kidneys usually last the longest.
Consider living donation
What does it mean to be a living donor?
Being a living donor means the donor chooses to give 1 of their 2 healthy kidneys to a person whose kidneys no longer work. Donating a kidney can help someone live longer.
Don’t people need 2 kidneys to live?
No. People can live long, healthy lives with 1 kidney. For donors and recipients, 1 kidney can do the work of 2 working kidneys if it’s working well.
Who can be a living donor?
Although the restrictions vary from transplant center to center, living donors are typically volunteers who:
- Are 18 years old or older.
- Are healthy and do not have kidney disease.
A living donor may be anyone—from family, friends, or neighbors of the kidney patient to a complete stranger. Donors do not have to be the same race, age, blood type, or sex as the kidney patient.
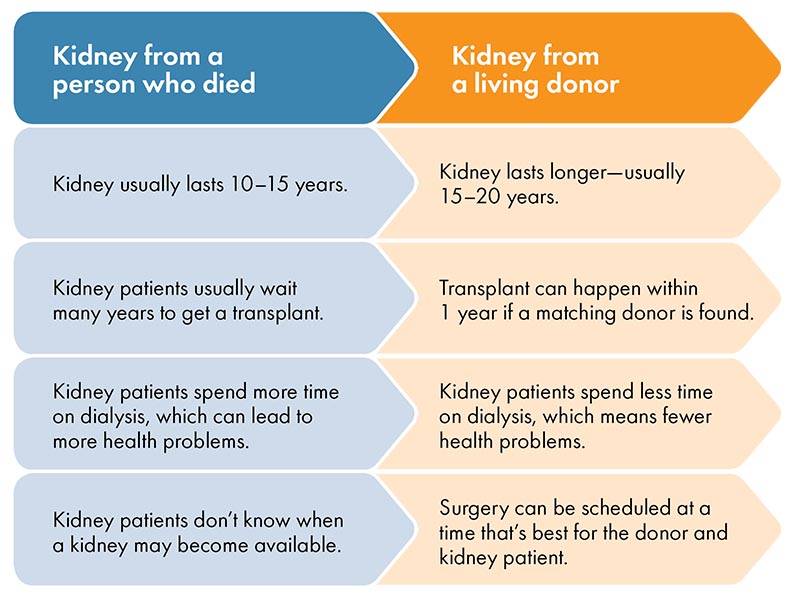
Why is a living donor transplant better than a deceased donor transplant?
There are many reasons why a kidney from a living donor is better than a kidney from someone who has died:
The living donor process:
Evaluation, surgery, and recovery
What is the donor evaluation process?
The donor evaluation process is a set of medical and psychological tests to make sure that the donor is healthy enough to have surgery and the donation is likely to work.
What kind of tests do donors need?
The medical team will compare the blood of the potential donor and kidney patient to see if they are a match. If they’re a match, the donor will get medical tests such as:
- Blood pressure checks
- Blood and urine tests
- Breast exam and Pap smear to test for cervical cancer (in women)
- Colonoscopy to test for colon cancer (in donors over age 50)
- An angiogram test to help doctors see the blood vessels of the kidney
- Chest x-rays
- Cardiac (heart) stress test
- Other tests if the tests above come back abnormal (unusual)
Some of the tests can be done locally or before coming into the transplant center. Donors also talk to a social worker or counselor who make sure they have a support system, such as family and friends, who can help them after the donation.
How long does the evaluation process take?
The donor’s evaluation can take several months, depending on the health of the donor and how quickly they can do the tests.
What if the donor wants to stop the process?
A person who’s being tested as a living donor can change their mind about donating at any point, for any reason—even on the day of surgery. There is no penalty for wanting to stop the process.
What is transplant surgery like for the donor?
The donor and kidney patient are admitted to the hospital the morning of the day of the surgery. Both surgeries happen at the same time and take 3–5 hours. The donor will get general anesthesia, which will put them to sleep and prevent pain. Doctors will put a small tube in their vein for fluids and medicines. They’ll also put a tube in their bladder after the surgery to measure how much urine they put out.
What are the 2 main types of surgery?
Laparoscopy: This surgery uses a wand-like camera placed in small cuts in the donor’s belly. It lets doctors view the kidney and take it out through a small cut. Doctors then close the cuts with stitches. The benefits of this type of surgery include:
- Shorter hospital stay
- Shorter recovery time
- Smaller cuts
- Fewer problems after surgery
Open surgery: Doctors cut open the donor’s belly to take out the kidney, then close the cuts with stitches.
After either type of surgery, doctors connect the donor’s kidney into the kidney patient’s body right away.
How painful is the surgery?
Donors usually feel the most pain the first week after surgery. They can take medicine for their pain. Many donors say that seeing the kidney patient start to feel better helps them forget about their own pain.
What happens to the donor’s kidney function during surgery and after they donate?
What is recovery like after donation and how long does it take?
Donors usually stay in the hospital for 1–2 days. After leaving the hospital, donors have to rest at home, usually for about a week, while their body begins to heal. Over time, they start to feel better and are able to do more. Most donors can drive and return to their normal lives in 4 weeks.
At the time the kidney is removed, the donor will lose half of their kidney function. Over time, the donor’s remaining kidney will get bigger to do the work of both kidneys.
How does the donor have to care for their health after donating?
Transplant centers follow up with donors for at least 2 years after donation to make sure that they’re healing well and are healthy. After they’ve recovered, donors return to the care of their regular doctor. They should have their blood pressure and kidney function checked regularly for the rest of their lives
Possible risks of living donation There are risks to all surgeries. There are medical, emotional, and financial risks for living donors. The transplant team keeps living donors as safe as possible. They will not let someone donate if they face any large risks. It’s very important living donors don’t feel pressured to donate. A Living Donor Advocate is a social worker, nurse, or doctor who protects the rights and health of living donors.
What are the medical risks of donor surgery?
Normally, doctors remove the kidney through an opening only a few inches long. If there are problems, the opening may have to be larger and recovery may take longer. Donors may have some short-term problems from surgery, such as:
- Bloating
- Feeling sick to their stomach
- Scars and pain
- Feeling tired and weak
More serious problems from surgery happen in less than 5% of donors (less than 1 in 20 donors). The surgical team does everything they can to avoid these problems. These could include:
- Problems from being put to sleep, such as confusion after surgery, pneumonia, stroke, or heart attack
- Infection
- Fever
- Bleeding and blood clots The risk of death is less than 3 in 10,000 donors—this is much less than 1% of donors.
Can living donors still have children after they donate?
Yes, both men and women can donate and still have children. Women should wait 1 year after donating before getting pregnant so that their bodies can fully heal.
What are the financial risks of living donation?
Medicare or the kidney patient’s private insurance will cover the donor’s medical costs. However, most insurance companies don’t cover:
- Time off from work and child care
- Gas or travel costs
- Meals
- Parking
- Hotel costs from donor testing, surgery, and recovery
Donation can sometimes change the donor’s ability to get or afford health, disability, or life insurance. Donors may also have issues getting work in military service, law enforcement, aviation, and fire departments.
What emotional risks are there for living donors?
It’s very important that donors don’t feel pressured to donate. Donors can stop the transplant at any time, even on the day of the surgery.
The donor’s relationship with the kidney patient might become strained if the kidney ever stops working.
Will a living donor have health problems after donating?
Most donors who follow a healthy lifestyle after surgery remain just as healthy after donation as people who have not donated. For most donors, the remaining kidney works fine for the rest of their lives.
Some kidney donors get high blood pressure or diabetes, which doctors can treat with medicine. People who donate a kidney have a very small chance of developing kidney failure. If it does happen, the donor is put at the top of the deceased donor waiting list to get a kidney transplant.
Women should talk with the transplant team about a small risk of high blood pressure during future pregnancies.
Most studies on the long-term outcomes of donors have followed donors for only the last 20 years. For this reason, there is little information about the 40–50 year outcomes from donors.
Living donors can help in many ways
There are many ways to donate.
- Directed donation: A living donor donates a kidney to a specific kidney patient.
- Non-directed donation: A living donor donates a kidney to someone in need, even though they don’t know the specific patient. The living donor may do this for personal or spiritual reasons. They can choose to donate to a single kidney patient or can join an exchange program to support many people getting a transplant.
Exchange programs make it possible to help more than 1 patient
Sometimes a donor isn’t a good match for the specific kidney patient they want to donate to. Even so, they can still help the patient they know get a living donor transplant.
An exchange program called a paired donation or donor chain makes it possible for 1 donor to help more than 1 kidney patient:
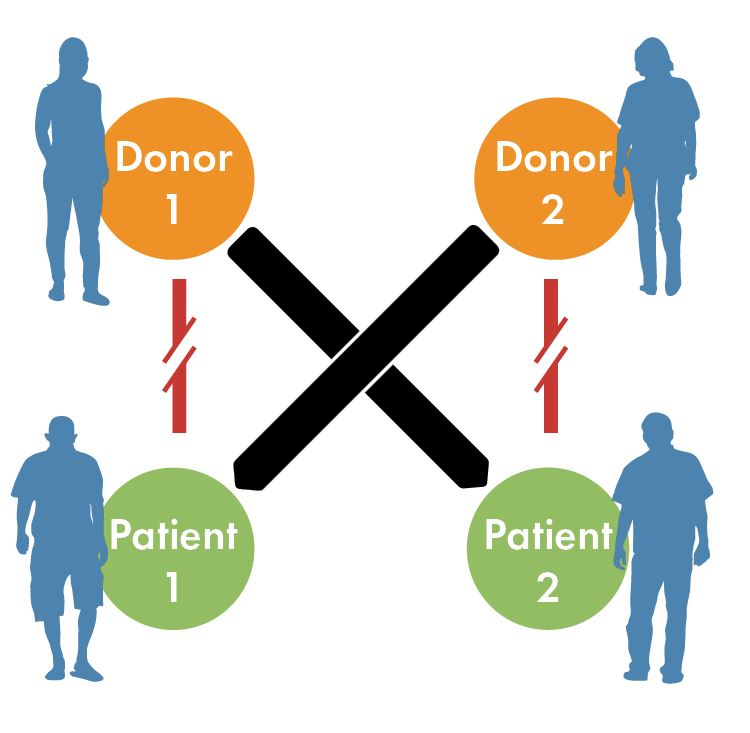
- Paired donations: A paired donation helps when 2 kidney patients have healthy donors who aren’t good matches for them. The 2 patients swap donors so each can get a kidney that’s a good match for them.
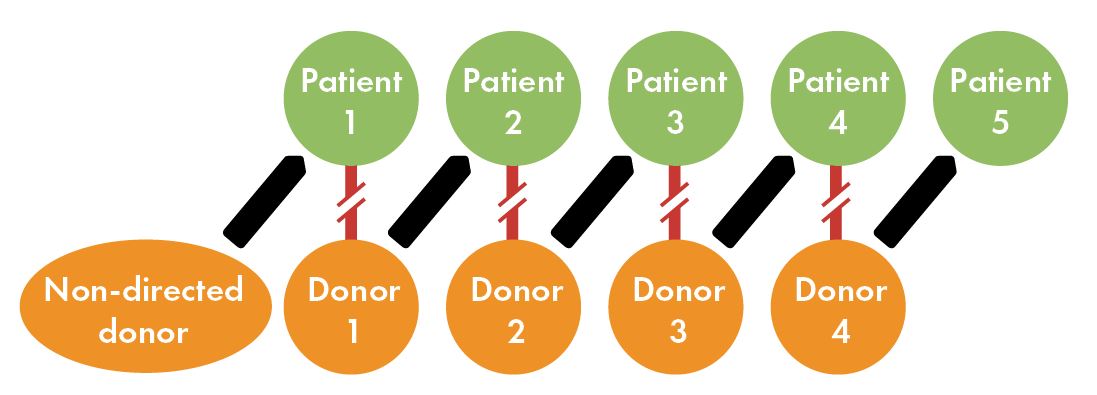
- Donor chains: A chain can help a group of kidney patients who have healthy donors that aren’t good matches. When a kidney patient gets a donor who isn’t a match, they may be linked to a group of patients who can switch donors around. Swapping donors helps the whole group, or chain, of kidney patients. Sometimes 20 or more kidney patients in a chain are able to get living donor transplants!