Written by Alexis Bobu, Scientific Writer, Houston Methodist Hospital Department of Surgery and J.C. Walter, Jr. Transplant Center
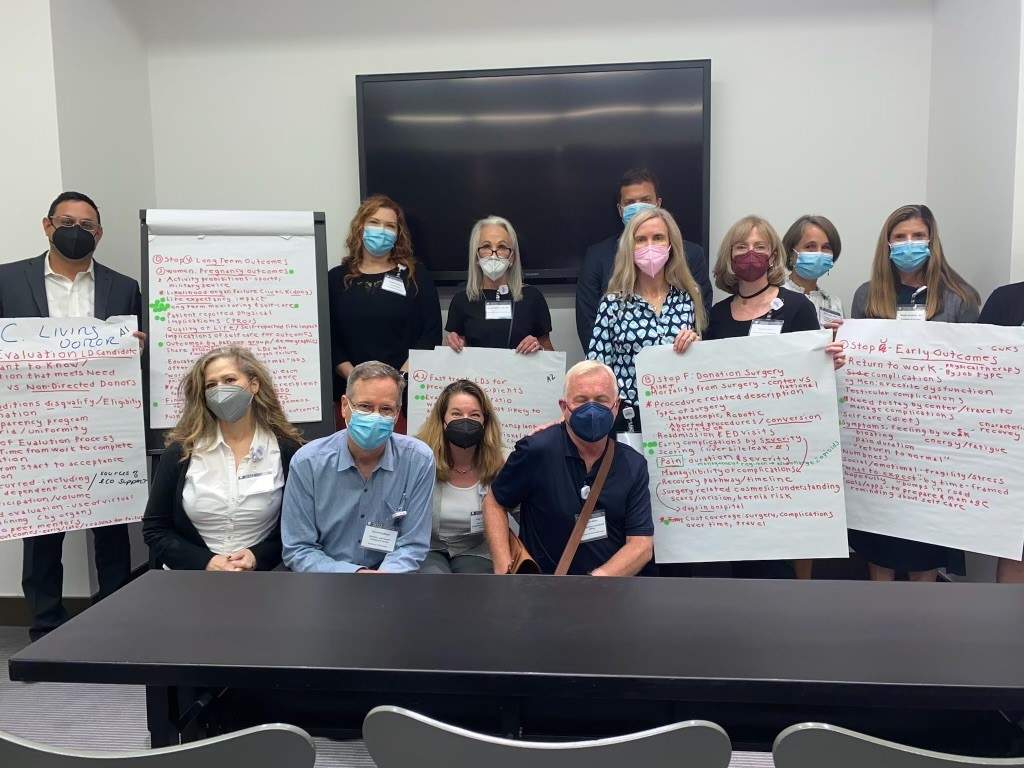
The Scientific Registry of Transplant Recipients (SRTR) hosted the People Driven Transplant Metrics Consensus Conference in Bloomington, Minnesota on July 18 – 20th, 2022 to develop priorities to expand transplant metrics to better include what is important to transplant patients, donors, and those that love them. For two days at the Mall of America, patients, living donors, caregivers, researchers, allied health professionals, physicians, and others came together to share their perspectives on this important question. What a powerful and important focus!
After the conference, Dr. Amy Waterman, Director of Patient Engagement, Diversity, and Education, for Houston Methodist Hospital’s Department of Surgery and J.C. Walter Jr. Transplant Center, met virtually with Mr. Jim Gleason and Ms. Lorrinda Gray-Davis, a heart and liver transplant recipient, respectively, representing the Transplant Recipients International Organization (TRIO), to reflect on key takeaways. All three agreed that hearing the different voices of the transplant community at one time was greatly beneficial and left them very hopeful. Lorrinda said, “I enjoyed hearing different stakeholders discuss what they valued because everyone had different opinions about the transplant journey, recommended measurement tools, and preferred metrics.”
Jim Gleason shared how he was impressed by how the SRTR conference leaders found ways to subsidize the costs for patients and their families who were attending in person by providing scholarships. He stated, “they’re recognizing that the patient really is the focus of a lot of these metrics. Many patients, like Jim, had the opportunity to attend virtually, to reduce their risk of contracting COVID-19.
The conference presented the process of pursuing and getting a transplant through the visual metaphor of a subway map, with colors indicating different stops and routes for patients and donors. Different providers and parts of the healthcare delivery system were visually presented in parts of the subway routes where they connected to the subway riders to facilitate transplants. Lorrinda commented that the subway analogy was outstanding, stating, “As a patient, there are a lot of things we don’t understand, but this gave us a better picture of what transplant looks like as a whole.” Dr. Waterman remarked how monumental the subway analogy was and said, “for the first time, the whole field started working off of one mapped-out visual, building out what was missing and naming how success could be measured.”
When it came to discussing improvements in person driven metrics, one takeaway was the importance of reframing metrics that might be upsetting to patients more positively. For example, one simple change could be made to the metric of organ failure, reversing metrics reporting how many transplants failed over 3 years to how many transplants were still working. Jim added to the conversation by saying, “as a mathematician, I love numbers and metrics, and changing the language to be more positive and supportive can be very impactful for the patient and doesn’t impact the scale because the meaning remains the same.”
Lorrinda also commented on how many patients are grappling with the two M’s related to ensuring their eligibility to get a transplant: Money and a positive Mental Health Evaluation. Financial challenges are common for transplant patients. Recommendations by transplant centers for individuals to fundraise to cover these costs seem impossible for many. Some also think that the psychiatrist is the sole decision-maker for transplant eligibility. Better education about all of the evaluation criteria, from health, to psychosocial factors, to financial eligibility, is needed.”
Moreover, Dr. Waterman stated that, “this conference really revealed that patients care about many other metrics that are currently not being measured by the SRTR.” Prioritized recommendations at the conference by their Working Group included metrics related to post-transplant survival for patients and long-term health data for living donors. Dr. Waterman noted that patients expressed the most interest in quality-of-life indicators and mental health metrics that assessed dimensions like depression and anxiety and ability to return to school or work after transplant. Lorrinda added that “mental health needs to be better addressed through Peer-to-Peer support groups rather than on Facebook. Facebook groups are more likely to lead patients to misinformation or misunderstandings as people communicate from all over the globe providing different diet recommendations, medications, and practices that may not always be true for an individual patient.”
In closing, Lorrinda mentioned that while there is now a subway map for transplant generally, the details should be further clarified by organ and donor type. All three conference attendees agreed that better education, in addition to metrics, was necessary to ensure that patients and families had what they needed. Lorrinda emphasized the need for education earlier saying, “it [education] needs to start with their primary care doctor, nephrologist, cardiologist, and hepatologist, that are all part of the transplant team. I believe some patients start the process too late and they don’t have a chance to get listed or recover.” With education being so important, Jim was excited to share that TRIO is considering adding educational resources and links to their website to help the transplant community as they did with their Post-Transplant Cancer Project, bringing hope and education to the field of transplant. Dr. Waterman added, “there’s a lot of work to be done at the SRTR level. But what came out of this conference was a clear commitment to expand metrics to better empower patients.”